The emergence of pediatric cancer AI predictions marks a significant breakthrough in oncology, especially for brain tumors like gliomas. Recent advancements in AI in pediatric oncology demonstrate that artificial intelligence tools can accurately forecast the risk of cancer relapse, as revealed by a groundbreaking study from Mass General Brigham. By analyzing multiple brain scans over time, this innovative approach outperforms traditional single-scan methods in predicting glioma recurrence, thus offering renewed hope for young patients and their families. Researchers have successfully implemented temporal learning in healthcare, which fine-tunes the AI’s ability to detect subtle changes, improving diagnostic accuracy to remarkable levels. Such developments in AI medical imaging not only enhance clinical decision-making but also pave the way for personalized treatment strategies that could revolutionize care for pediatric gliomas.
The field of pediatric oncology is witnessing a transformative shift with the integration of advanced machine learning techniques that enable precise predictions regarding childhood cancer outcomes. Scholars and healthcare professionals are examining novel methodologies that leverage AI for predicting the likelihood of disease recurrence in children suffering from brain tumors, such as pediatric gliomas. Current studies are increasingly focused on the utilization of temporal analysis to enhance the reliability of diagnostic imaging over time. This innovative approach allows clinicians to monitor progression and respond proactively to potential relapses, thereby tailoring care to individual patient needs. As research continues to evolve, the potential of AI-driven insights in managing pediatric cancer becomes more evident, promising significant improvements in treatment trajectories.
Revolutionizing Pediatric Oncology with AI
Artificial Intelligence is making significant strides in the field of pediatric oncology, transforming how healthcare professionals predict and manage diseases. The integration of AI tools in predicting pediatric cancer outcomes has ushered in a new era of precision medicine. With advancements such as temporal learning, AI can analyze vast amounts of medical imaging data, providing insights that are not easily discernible through traditional methods. This capability allows for more personalized treatment plans and better patient outcomes, reducing the emotional and physical burden on young patients and their families.
As AI technology continues to evolve, its applications in pediatric oncology promise a future where early detection and tailored treatment become the standard. Reports indicate that tools developed to predict glioma recurrence risk through comprehensive analysis of multiple scans have shown improved accuracy compared to conventional single-scan evaluations. By harnessing the predictive power of AI, healthcare teams can make more informed decisions and optimize care pathways, ensuring that children receive the most effective treatment with minimal distress.
The Impact of Temporal Learning in Predicting Tumor Recurrence
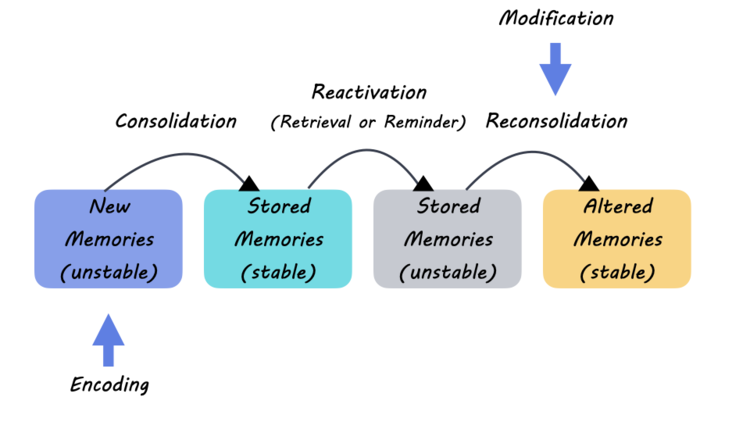
Temporal learning is a pioneering approach that represents a significant breakthrough in medical imaging for pediatric gliomas. Unlike traditional models that evaluate and learn from isolated scans, temporal learning takes into account the sequence of images collected over time, allowing for a more comprehensive understanding of tumor dynamics. This method enhances the AI’s ability to identify subtle, progressive changes that may indicate potential relapse, offering higher predictive accuracy. For glioma patients, this translates into improved monitoring protocols and reduces unnecessary imaging for those at lower risk.
The integration of temporal learning into pediatric cancer prediction models can dramatically enhance the prognosis framework for young patients. Researchers have demonstrated that this advanced approach can deliver up to 89 percent accuracy in predicting relapse, significantly surpassing the predictive capabilities based solely on single images. By focusing on the trajectory of tumor evolution, this technique not only aids in recognizing patients at high risk for recurrence but also supports healthcare providers in crafting proactive treatment strategies that can mitigate more severe complications.
AI Medical Imaging and Its Role in Pediatric Cancer Care
AI medical imaging revolutionizes how pediatric cancers are diagnosed and monitored, particularly in conditions like gliomas. With the capacity to process and analyze thousands of brain scans efficiently, AI provides healthcare professionals a powerful tool to detect subtle changes over time that human analysis may overlook. Enhanced imaging capabilities not only streamline clinical workflows but also lead to accurate diagnoses and timely interventions, reducing the psychological toll on young patients and their families.
Moreover, the implications of AI in medical imaging extend beyond initial diagnosis; they encompass the entire patient care continuum. By implementing AI-driven methodologies, healthcare providers can establish more effective follow-up protocols, tailoring surveillance strategies to individual risk levels. This proactive and personalized approach in pediatric oncology is crucial in enhancing patient outcomes and ensuring that children receive the right care at the right time, ultimately showcasing the profound potential of AI in transforming pediatric cancer management.
Understanding Pediatric Gliomas: A Complex Challenge
Pediatric gliomas are a diverse group of brain tumors, presenting unique challenges in terms of treatment and prognosis. These tumors can range from benign to highly malignant, with varying degrees of recurrence, thus requiring a nuanced understanding and a multidisciplinary treatment approach. Early detection and continuous monitoring are critical for improving patient outcomes, which makes the integration of advanced AI tools, such as those used in predicting recurrences, essential. The complexities associated with pediatric gliomas necessitate ongoing research and innovation in treatment protocols.
Equipped with sophisticated AI analysis, healthcare providers can better predict the behavior of pediatric gliomas. For instance, by utilizing multi-scan data through temporal learning, researchers are able to gather insights about tumor recurrence and develop strategies tailored to each patient’s needs. This not only enhances the overall management of gliomas but also fosters collaboration among oncologists, radiologists, and researchers to advance the understanding of pediatric brain tumors, ultimately leading to more effective therapeutic options.
The Future of Pediatric Cancer Management with AI
Looking ahead, the integration of AI in pediatric cancer management is set to redefine care standards. As emerging technologies continue to refine predictive models, healthcare providers can look forward to personalized treatment paths informed by reliable data analytics. With AI models showing promise in accurately predicting pediatric cancer recurrence, there is potential to significantly improve therapeutic outcomes and optimize resource allocation within healthcare systems.
Furthermore, clinical trials utilizing AI-informed risk predictions could serve as pivotal turning points in pediatric oncology. By assessing the efficacy of these innovative tools, healthcare professionals can uncover strategies that minimize invasive procedures for at-risk patients, leading to less psychological and physical strain. The future of pediatric cancer treatment relies heavily on the advancements in AI and the commitment to leveraging these technologies for enhanced patient care.
Clinical Trials: Advancing AI Tools in Pediatric Oncology
Clinical trials play a crucial role in validating the effectiveness of new AI tools in pediatric oncology. As researchers explore the potential of AI in predicting glioma recurrence, these trials will be essential for assessing how well these technologies can transition from theoretical models to real-world applications. Such pivotal research will not only inform clinical practice but will also contribute to the regulatory landscape surrounding AI usage in healthcare.
Conducting rigorous clinical trials will help establish benchmarks for AI applications in pediatric cancer management. This includes evaluating the accuracy and reliability of different AI models in predicting patient outcomes, and their impact on treatment decisions. Ultimately, successful trials could pave the way for broader acceptance and integration of AI technologies into standard protocols, fostering a more responsive and adaptive pediatric oncology framework.
Collaboration Between AI Experts and Healthcare Professionals
The collaboration between AI experts and healthcare professionals is critical in advancing the application of artificial intelligence in pediatric oncology. By working together, these two fields can bridge the gap between machine learning technology and practical healthcare solutions. The insights gained from oncologists and radiologists are essential in fine-tuning AI algorithms, ensuring they are aligned with clinical needs and expectations.
Moreover, effective collaboration opens pathways for interdisciplinary research, driving innovation and addressing the complexities surrounding pediatric cancers. By leveraging collective expertise, the development of AI tools can focus on improving accuracy in predictions of glioma recurrence and enhancing treatment pathways. This teamwork not only accelerates the integration of AI in healthcare but also fosters a culture of continuous learning and adaptation among clinical practitioners.
Potential Challenges in Implementing AI in Pediatric Oncology
While the prospects of AI in pediatric oncology are exciting, there are inherent challenges that need careful consideration. One significant concern is the quality and diversity of data used to train AI models. Ensuring that the datasets are representative of the population can help prevent biases that may lead to inaccurate predictions. Additionally, the reliance on machine learning can create challenges in clinical settings where clinicians must interpret AI-generated outcomes accurately.
Another challenge lies in the acceptance of these advanced technologies among healthcare professionals and families. Educating stakeholders about the benefits and limitations of AI tools in managing pediatric gliomas is essential. As the field advances, fostering trust and understanding will be vital in integrating AI solutions into everyday clinical practices while addressing ethical considerations surrounding data privacy and informed consent.
Emerging Technologies in Pediatric Cancer Research
The landscape of pediatric cancer research is continually evolving, driven by the rapid advancements in technology. Emerging technologies, particularly in the realm of artificial intelligence, are opening new avenues for exploring treatment options and understanding disease mechanisms. Research initiatives focusing on AI-assisted imaging techniques are at the forefront of this evolution, offering innovative methods for predicting and managing pediatric cancers with greater accuracy and efficiency.
The exploration of these cutting-edge technologies promises to enhance our understanding of complex conditions like gliomas. For instance, researchers are leveraging AI tools for multifaceted analyses that include genetic profiling and imaging data, which can lead to more tailored therapeutic approaches for young patients. As these technologies mature, they will form the foundation for transformative changes in how pediatric cancers are treated, ultimately resulting in improved patient outcomes.
Frequently Asked Questions
What are pediatric cancer AI predictions and how do they work?
Pediatric cancer AI predictions involve the use of artificial intelligence to analyze medical imaging data and other relevant factors to forecast the likelihood of cancer recurrence in children. By utilizing techniques such as temporal learning, these AI tools can evaluate multiple brain scans taken over time to identify patterns that traditional methods may miss, improving accuracy in predicting issues such as glioma recurrence.
How does AI improve predictions for pediatric gliomas specifically?
AI enhances predictions for pediatric gliomas by assessing a series of brain scans instead of relying on single images. This method, known as temporal learning, allows the AI to detect subtle changes over time, leading to a more reliable assessment of recurrence risk for these types of tumors.
What is the significance of temporal learning in AI for pediatric cancer predictions?
Temporal learning is significant in pediatric cancer predictions because it trains AI models to synthesize and analyze data from multiple imaging sessions over time. This approach has been shown to improve the accuracy of predicting relapse risks in pediatric gliomas, transitioning from traditional single-scan predictions that are often unreliable.
Can AI tools accurately predict glioma recurrence in pediatric patients?
Yes, AI tools have demonstrated the ability to predict glioma recurrence in pediatric patients with an accuracy ranging from 75 to 89 percent when using temporal learning to analyze multiple MR scans. This is significantly higher than predictions made from solitary images, thus highlighting the power of AI in pediatric oncology.
What potential benefits do pediatric cancer AI predictions offer?
Pediatric cancer AI predictions can lead to numerous benefits, including reducing the frequency of unnecessary imaging for low-risk patients, providing more targeted therapies for high-risk cases, and decreasing the overall stress and burden on families by improving the precision of monitoring and treatment strategies.
How is AI being utilized in pediatric oncology research?
AI is being utilized in pediatric oncology research by analyzing large datasets, including MRI scans of brain tumors, to uncover patterns that assist in predicting cancer outcomes. This application not only aids in understanding recurrence risks for pediatric cancers like gliomas but also enhances personalized treatment approaches.
What are the challenges in implementing AI predictions in pediatric oncology?
Challenges in implementing AI predictions in pediatric oncology include the need for further validation of AI models across diverse clinical settings, ensuring the accuracy of predictions before clinical application, and addressing potential ethical concerns regarding data privacy and the reliance on machine learning outcomes over traditional clinical judgment.
What research has been done on AI predictions for pediatric gliomas?
Recent research led by investigators from Mass General Brigham has focused on the development of AI tools that utilize temporal learning to effectively predict the risk of glioma recurrence in pediatric patients. Their findings, published in The New England Journal of Medicine AI, indicate significantly improved prediction accuracy compared to traditional methods.
How might AI be integrated into clinical trials for pediatric cancer treatment?
AI may be integrated into clinical trials for pediatric cancer treatment by evaluating patient responses to different therapies based on AI-driven predictions of relapse risk. This could allow for personalized treatment plans, minimizing unnecessary procedures for lower-risk patients while optimizing care for those at higher risk.
What future developments can we expect in pediatric cancer AI predictions?
Future developments in pediatric cancer AI predictions may include advanced algorithms that incorporate more data points, enhanced imaging technologies, and broader clinical applications. Researchers aim to refine these AI tools to further improve accuracy and integrate them into routine clinical practice for pediatric oncology.
| Key Point | Details |
|---|---|
| AI Predicts Relapse Risk Better | AI tool shows improved prediction accuracy for pediatric cancer recurrence compared to traditional methods. |
| Research Background | Study conducted by researchers from Mass General Brigham and Boston Children’s Hospital, published in The New England Journal of Medicine AI. |
| Study Contributions | Collected nearly 4,000 MR scans from 715 pediatric patients using innovative temporal learning techniques. |
| Effectiveness of Temporal Learning | 75-89% accuracy in predicting relapse, outperforming traditional methods which approximate 50% accuracy. |
| Future Applications | Aim to conduct clinical trials to implement AI findings and improve patient care. |
Summary
Pediatric cancer AI predictions have the potential to revolutionize how we assess relapse risks in young patients. With the innovative use of AI tools, researchers have significantly improved the accuracy of relapse predictions for pediatric glioma patients. The study highlights the importance of analyzing multiple brain scans over time, offering hope for enhanced monitoring and treatment strategies that could lead to better outcomes for children facing these critical health challenges.