Pediatric brain cancer prediction is a groundbreaking field that harnesses the power of advanced technology to foresee potential relapses in young patients afflicted with tumors like gliomas. A recent study reveals that AI predictive tools significantly outperform traditional methods in accurately forecasting the risk of cancer recurrence, thereby easing the considerable pressure faced by families. Utilizing sophisticated algorithms, the research emphasizes the analysis of multiple MRI brain scans over time, pushing the boundaries of pediatric cancer treatment to new heights. These findings highlight the importance of temporal learning in AI, which allows for a more nuanced understanding of tumor development and recurrence patterns. As a result, healthcare providers can tailor follow-up care and intervention strategies, dramatically improving outcomes for children battling brain cancer.
In the realm of childhood oncology, the forecast and management of brain neoplasms, specifically pediatric gliomas, stand as a pivotal concern. The innovative approaches in examining the likelihood of tumor recurrence by leveraging artificial intelligence not only enhance prediction accuracy but also redefine the standards of care in pediatric oncology. Through the integration of advanced imaging techniques, such as sequential MRI brain assessments, medical professionals can derive vital insights into the progression of these malignancies. The principles of predictive analytics in this context promise to alleviate the emotional and physical burdens on young patients and their families alike. Ultimately, the evolution of predictive modeling marks a significant step toward personalized medicine for childhood brain tumors.
Understanding Pediatric Brain Cancer Recurrence Risks
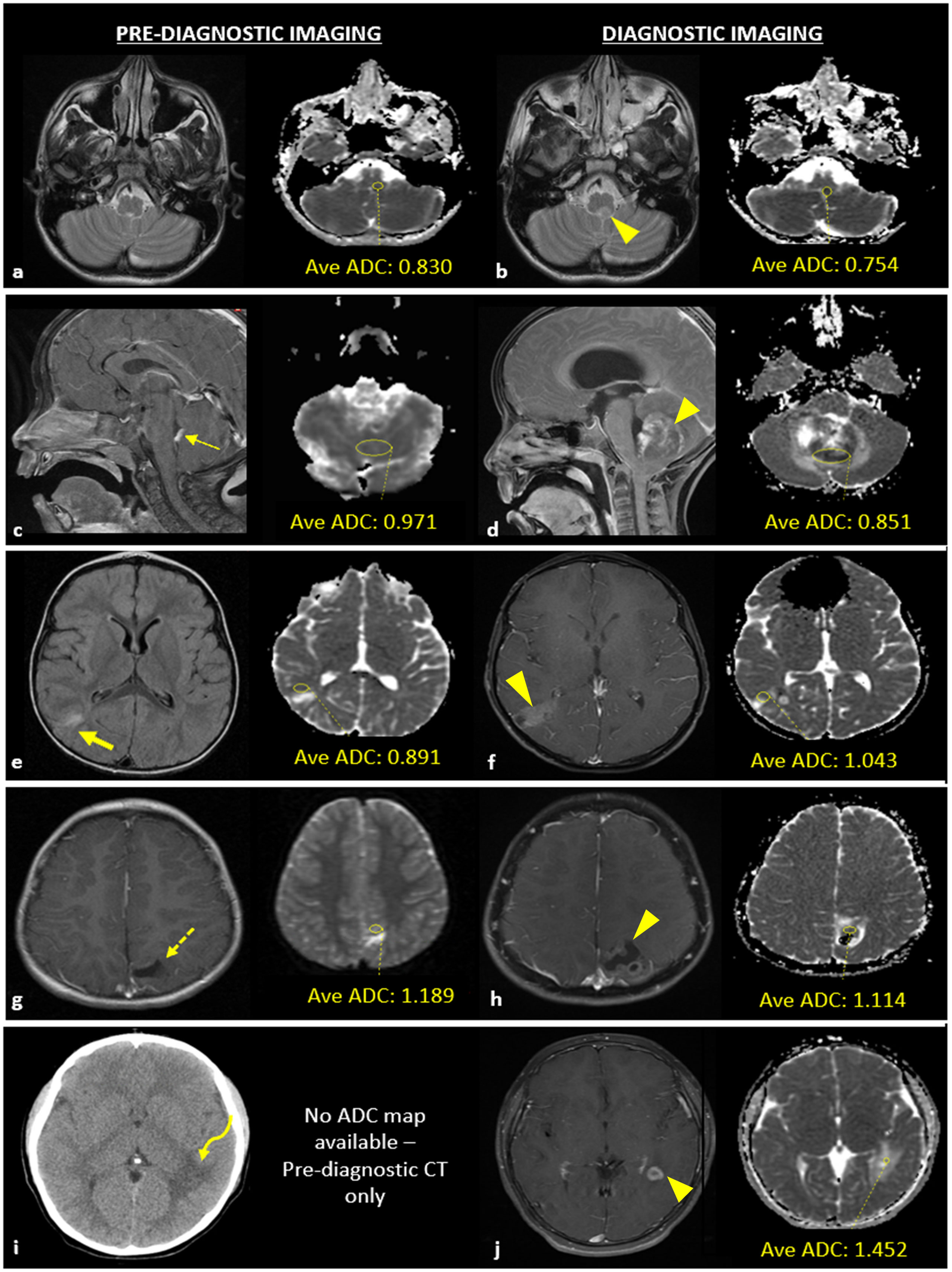
Pediatric brain cancer, particularly gliomas, presents unique challenges in predicting an individual’s risk of recurrence. Traditional methods relied heavily on one-off MRI scans, often resulting in uncertainty and anxiety for families. This is where the innovative use of AI predictive tools comes into play. By analyzing multiple MRI brain scans over time, these tools can highlight subtle changes in the brain’s condition that may indicate a higher risk of relapse, drastically improving the precision of forecasts.
In a groundbreaking study from Mass General Brigham, researchers demonstrated that AI-powered tools could predict recurrence risks with significant accuracy—up to 89%—outperforming traditional methods by a substantial margin. The shift from a reliance on individual scans to a comprehensive analysis that includes temporal learning allows healthcare providers to make informed decisions about post-surgery monitoring, potentially reducing the emotional and physical stress placed on young patients and their families.
The Role of AI in Pediatric Cancer Treatment
Artificial intelligence is reshaping pediatric cancer treatment, especially by enhancing the methods through which physicians assess the risk of glioma recurrence. The study conducted at Mass General Brigham showcased how AI can synthesize data from extensive collections of MRI brain scans, developing robust predictive models that inform treatment protocols. By employing temporal learning, a technique less frequently utilized in medical imaging, the AI learns from a sequence of scans, becoming more attuned to the fluctuations in a patient’s condition over time.
Incorporating AI tools into pediatric cancer treatment can facilitate personalized care strategies. Children identified as being at high risk of glioma recurrence can be steered towards proactive treatments, which may include targeted therapies administered alongside traditional modalities. This tailored approach signifies a shift towards utilizing advanced technologies, potentially offering better outcomes while lowering the burden of frequent imaging on patients.
AI Predictive Tools and Their Impact on Imaging Frequency in Pediatric Care
AI predictive tools are transforming how healthcare providers monitor pediatric brain cancer patients post-treatment. With the ability to analyze multiple MRI scans over time, these tools can ascertain recurrence risks far more accurately than conventional methods, significantly influencing the frequency of necessary follow-ups. For instance, the AI analyzed in the Mass General Brigham study distinguished between low- and high-risk patients effectively based on subtle changes captured in sequential imaging.
Through the integration of AI prognostics, physicians can allocate resources more efficiently, focusing on patients who require closer monitoring and reducing the anxiety associated with unnecessary imaging for those at lower risk. This not only streamlines clinical workflows but also paves the way for innovative approaches to manage pediatric gliomas, thereby enhancing overall treatment efficacy and patient experience.
MRI Brain Scans: The Traditional Approach to Monitoring
For years, MRI brain scans have been the cornerstone of monitoring pediatric patients with gliomas, especially following surgical interventions. However, this approach is not without its drawbacks. Traditional single-scan analysis often leaves much to be desired in terms of predictive accuracy, leading to uncertainty in clinical decision-making. Consequently, patients frequently undergo rigorous imaging schedules, which can be both physically taxing and emotionally burdensome for young children and their families.
The traditional reliance on these singular assessments is being challenged with the advent of AI-driven predictive analysis. By capturing and interpreting data from multiple scans over time, researchers can leverage these insights to shift from merely reactive to proactive patient management in pediatric cancer care. This represents a significant leap towards a more patient-centered approach, potentially reducing the need for unnecessary procedures while equipping clinicians with sharper insights into recurrence risks.
Temporal Learning in AI and Its Advantages
Temporal learning is a novel concept being integrated into AI models for predicting pediatric brain cancer recurrence, especially for gliomas. Unlike traditional training methods that focus on static images, temporal learning evaluates a sequence of scans, allowing the algorithm to recognize patterns and changes indicative of disease progression or stability. This multifaceted approach enhances the model’s predictive capabilities, yielding results that demonstrate a marked increase in accuracy when forecasting potential cancer relapses.
Implementing temporal learning within clinical practice can revolutionize how oncologists approach follow-up care for children post-glioma surgery. With improved accuracy, clinicians can tailor their monitoring strategies, pivoting quickly based on AI-driven insights. This innovation not only promises to enhance patient outcomes but can also lead to more effective allocation of healthcare resources, ensuring that high-risk patients receive the focused care they need.
The Future of Pediatric Brain Cancer Research
The future of pediatric brain cancer research is being shaped by technological advancements such as AI and its application in predictive analysis. The encouraging results from the recent study underscore the potential for AI predictive tools to transform patient monitoring and care standards. As researchers continue to refine these predictive models, the hope is that they will lead to groundbreaking insights that can directly impact treatment protocols and improve survival rates for children afflicted with gliomas.
Ongoing studies and clinical trials will be vital in validating AI’s predictions across diverse populations and settings. By harnessing the vast potential of AI, the medical community can make strides towards personalized medicine, where treatment plans are informed by individual patient data rather than generalized models. This evolution represents a prospective shift in pediatric cancer care, advocating for innovations that prioritize both accuracy and patient well-being.
Addressing the Challenges in Pediatric Cancer Monitoring
Monitoring pediatric brain cancer patients, particularly those with gliomas, presents unique challenges. Frequent MRIs can cause anxiety and discomfort for young children, and traditional methods often lack the precision needed to predict recurrence effectively. These challenges necessitate the urgent integration of advanced technologies such as AI predictive tools, which have shown promise in transforming how these vulnerabilities are addressed.
By utilizing AI models that employ temporal learning, the healthcare community stands to enhance monitoring processes. Improved accuracy in predicting glioma recurrence can lead to a reduction in unnecessary scans, easing the emotional burden on families while ensuring that high-risk patients receive important interventions in a timely manner. This forward-thinking approach highlights the need to innovate traditional monitoring practices with cutting-edge solutions.
Personalized Treatment Plans for Pediatric Glioma Patients
Pediatric glioma patients can greatly benefit from personalized treatment strategies that utilize AI-driven insights to forecast their risk of recurrence. By leveraging data obtained from a series of brain scans, physicians can tailor post-operative care to better suit the specific needs of each child. Personalization in treatment plans not only improves overall patient outcomes but also increases the engagement of families in the treatment journey.
As research continues to highlight the effectiveness of AI in predicting glioma relapse risks, healthcare providers are better equipped to have informed discussions with families regarding treatment options. This collaborative approach fosters a supportive environment wherein families feel empowered, and the focus can shift to holistic care that addresses both medical and emotional needs during challenging times.
Conclusion: Embracing AI for Improved Pediatric Cancer Care
The integration of AI predictive tools in pediatric brain cancer care marks a pivotal moment in enhancing treatment and monitoring protocols for children with gliomas. As studies demonstrate the efficacy of these tools, particularly when trained on multiple MRI brain scans through temporal learning, it’s clear that the future of pediatric oncology is bright with technological innovation. AI brings with it the potential not only to improve predictive accuracy but also to alleviate the burdens associated with traditional monitoring methods.
In conclusion, by embracing these advancements in AI, healthcare professionals can work towards providing tailored, patient-centered care that prioritizes the unique challenges faced by pediatric brain cancer patients. The commitment to ongoing research and clinical validation will further establish AI as a cornerstone of modern pediatric oncology, paving the way for a future where outcomes are significantly enhanced and the journey of care is less fraught with unnecessary stress.
Frequently Asked Questions
How do AI predictive tools enhance pediatric brain cancer prediction?
AI predictive tools significantly improve pediatric brain cancer prediction by analyzing multiple MRI brain scans over time. Traditional methods often rely on single images, but AI uses temporal learning to assess changes across scans, leading to more accurate predictions of glioma recurrence and better patient care.
What role do MRI brain scans play in pediatric brain cancer prediction?
MRI brain scans are crucial in pediatric brain cancer prediction as they provide detailed images of brain tumors in children. Recent studies show that AI tools analyzing these scans can predict the risk of glioma recurrence more accurately than traditional methods, offering hope for improved treatment strategies.
What is temporal learning in AI and how does it relate to pediatric cancer treatment?
Temporal learning in AI refers to the technique of training models using sequential MRI brain scans acquired over time. This approach allows the AI to learn subtle changes that indicate possible glioma recurrence, thus aiding pediatric cancer treatment by identifying high-risk patients earlier for targeted interventions.
Can AI help predict glioma recurrence in pediatric patients?
Yes, AI has proven capable of accurately predicting glioma recurrence in pediatric patients. By utilizing advanced algorithms and analyzing multiple brain scans over time, AI tools can predict recurrence within a year post-treatment, enhancing treatment decisions and improving patient management.
What impact do AI predictive tools have on the care of pediatric patients with brain tumors?
AI predictive tools can transform the care of pediatric patients with brain tumors by providing precise risk assessments for glioma recurrence. This can lead to reduced frequency of stressful follow-up MRI brain scans for lower-risk patients and prompt treatments for those at higher risk, ultimately improving overall patient outcomes.
How effective is AI in predicting relapse risk in pediatric brain cancer cases?
AI has shown to be highly effective in predicting relapse risk in pediatric brain cancer cases, with studies indicating an accuracy rate of 75-89% when using temporal learning on multiple MRI brain scans. This represents a substantial improvement over traditional prediction methods, which have only about 50% accuracy.
What future developments are anticipated for AI tools in pediatric brain cancer prediction?
Future developments in AI tools for pediatric brain cancer prediction include further validation across diverse clinical settings and the initiation of clinical trials. Researchers hope to refine AI models to enhance accuracy and ultimately integrate them into standard care for better management of glioma recurrence.
| Key Point | Details |
|---|---|
| AI Tool Predictions | An AI tool has been developed that predicts the risk of relapse in pediatric brain cancer patients more accurately than traditional methods. |
| Study Findings | The study showed that AI could predict recurrence rates of gliomas with 75-89% accuracy based on multiple brain scans. |
| Temporal Learning Technique | The researchers used a new technique called temporal learning, which examines changes in brain scans over time, to improve predictions. |
| Impact on Treatment | This AI-driven approach might reduce unnecessary imaging procedures for low-risk patients and allow for early intervention in high-risk cases. |
| Future Research | Further validation is needed before clinical application, with intentions to conduct clinical trials utilizing AI-based predictions. |
Summary
Pediatric brain cancer prediction is revolutionizing the way healthcare providers assess the risk of recurrence in children suffering from brain tumors. By harnessing the power of artificial intelligence, particularly through innovative techniques like temporal learning, predictions regarding relapse can be made with remarkable accuracy. This advancement not only aids in identifying high-risk patients earlier but also significantly enhances the overall treatment strategy, ultimately aiming to reduce the psychological burden on young patients and their families.