CRISPR gene editing stands at the forefront of modern biotechnology, revolutionizing the way we approach genetic ailments and treatments. By enabling precise modifications at the genetic level, this groundbreaking CRISPR technology offers potential cures for diseases like sickle cell through innovative gene therapy. However, the ethical implications surrounding gene editing ethics raise significant questions about our responsibility to alter human genetics. Discussions on bioethics in medicine highlight the urgent need to consider health equity in gene therapy, especially as treatment access could benefit some while leaving others behind. As we tread this complex landscape, the promise of CRISPR gene editing invites a careful examination of its societal impact and the moral dilemmas it presents.
Genetic modification techniques are rapidly evolving, with CRISPR gene editing emerging as a pivotal player in the fight against hereditary diseases. This technology allows scientists to make targeted alterations in the genetic code, promising transformative outcomes such as potential cures for conditions like sickle cell anemia. Nevertheless, the intersection of innovative gene therapy and ethical considerations becomes increasingly crucial as we ponder questions related to genetic equity and the long-term effects of such alterations on human diversity. The discourse around bioethics and the responsibilities of altering our genetic traits has never been more vital. With advancements in this field, we must focus not only on the possibilities but also on ensuring fair access and addressing the moral concerns that arise from these powerful genetic tools.
The Promise of CRISPR for Treating Sickle Cell Disease
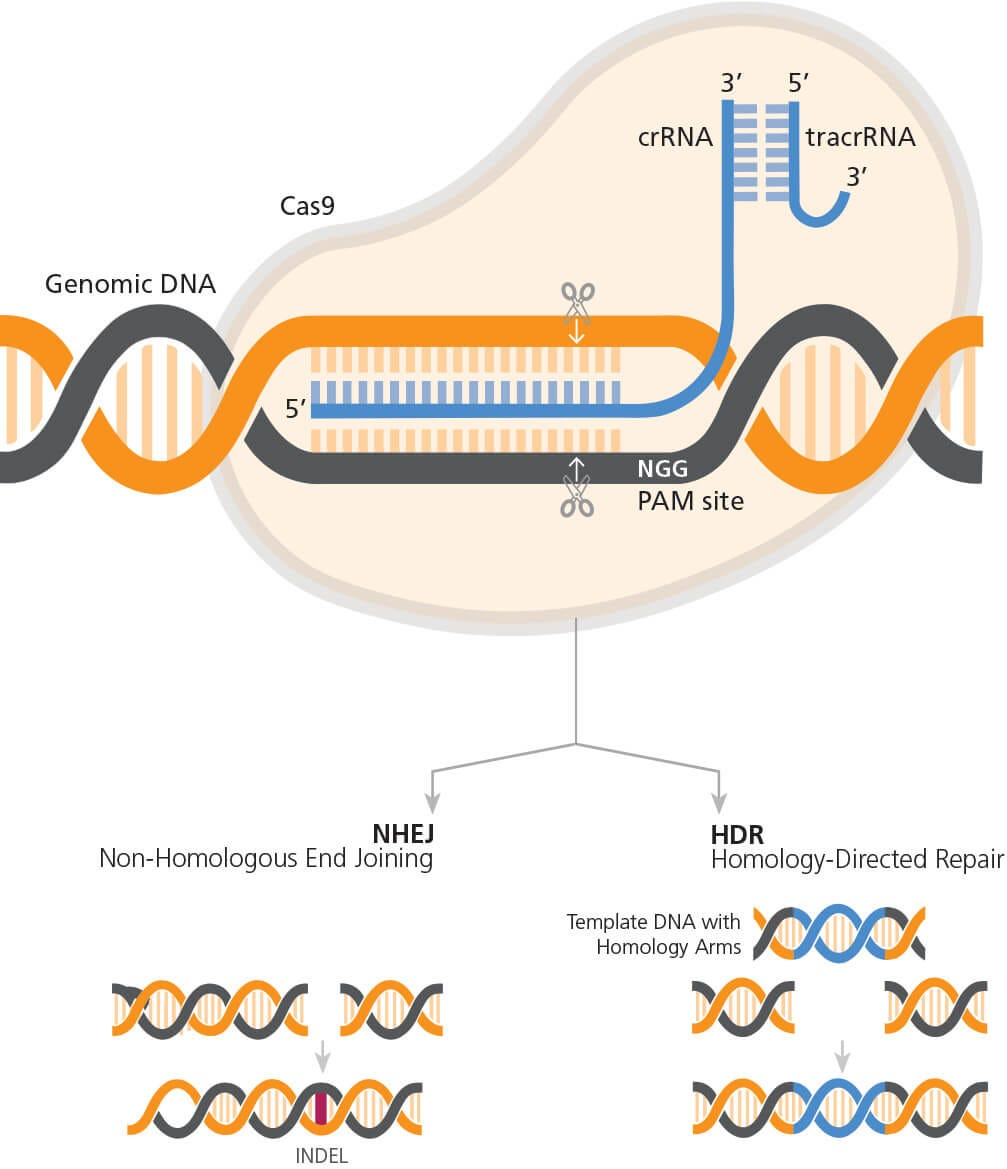
CRISPR gene editing holds significant promise for the treatment of sickle cell disease, allowing for revolutionary changes in how we approach hereditary disorders. With the ability to edit the genes within a person’s own cells, scientists can target the mutations that cause sickle cell anemia. As highlighted during a recent talk by Neal Baer, the potential to alleviate suffering and provide a cure represents a beacon of hope for thousands affected by this condition. Patients who once faced painful crises and potential strokes now see a pathway to health through gene therapy, thanks to advancements in CRISPR technology.
However, the optimism surrounding CRISPR is tempered by ethical questions that demand careful consideration. For instance, while the current focus might be on severe conditions like sickle cell anemia, we must grapple with whether gene editing should extend to traits or conditions that do not significantly impair life, such as certain syndromes. This discussion inevitably fuels debates about what it means to alter human genetics and the potential slippery slope of ‘designer babies’, where parents might choose genetic traits based on personal preference, rather than necessity.
Ethical Implications of Gene Editing in Medicine
The ethical landscape of gene editing is complex and fraught with challenges. As discussed by Baer and bioethics expert Rebecca Brendel during their talk, gene editing raises questions about who has the authority to make decisions regarding genetic changes. The line between therapeutic intervention and enhancement becomes blurred, as society must decide which conditions warrant intervention. The presence of CRISPR technology complicates this further, as it provides unprecedented access to the building blocks of life.
Additionally, the issues of equity and justice are paramount in the discourse surrounding gene therapy. The astronomical costs associated with CRISPR treatments, such as the approximately $2.2 million for curing sickle cell disease, highlight concerns about access. The potential for health disparities to widen if only the affluent can afford these innovations leads to calls for a more equitable approach to genetic medicine. Stakeholders in health equity must work towards ensuring that advancements do not leave marginalized communities behind.
Exploring Health Equity in Genetic Therapy
The advancement of gene editing technology brings exciting possibilities for improving human health, but it also shines a light on the urgent need for health equity in gene therapy. With the power of CRISPR, treatments for conditions that disproportionately affect marginalized populations, like sickle cell disease, may lead to significant improvements in quality of life. However, if these treatments remain accessible only to a privileged few, we risk exacerbating existing inequalities in healthcare.
To address these disparities, it’s essential to adopt a framework of health justice as highlighted by Brendel in her discussions. This involves not just making innovative treatments available but also ensuring they are affordable and accessible to all who need them. Policymakers, healthcare providers, and bioethicists must collaborate to create an equitable distribution of gene therapy resources, focusing on both the technological advancements and the socio-economic barriers that impact healthcare access.
CRISPR Technology: A Double-Edged Sword
While CRISPR technology heralds a new era of possibilities in gene therapy, it is essential to recognize its potential pitfalls. As discussed in the context of ethical considerations, the capacity to alter genetic codes brings forth significant risks, including unintended consequences that may arise from gene editing. The modification of a single gene can lead to unanticipated interactions within the genome, complicating our understanding of genetic health and disease.
Moreover, as we explore the boundaries of gene editing, we must address the regulatory gaps that exist globally. Nations vary in their laws regarding genetic modifications, and this inconsistency raises legitimate concerns over bioethics in medicine. The possibility of misuse or the lack of oversight, particularly in countries where regulations are lax, underscores the critical need for a comprehensive international framework governing CRISPR utilization.
The Role of Bioethics in Gene Editing Discussions
Bioethics plays a crucial role in shaping the dialogue surrounding gene editing technologies like CRISPR. Experts like Rebecca Brendel emphasize that as we venture into uncharted territories of genetic modification, we must create frameworks that ensure ethical standards are upheld. This includes ongoing discussions on issues such as consent, the rights of potential patients, and the implications of genetic alterations on future generations.
Further, bioethics in medicine brings attention to the societal systems that influence healthcare access and decision-making. Advances in gene editing should not only focus on the technological aspects but also how these innovations intersect with justice, equity, and the values of communities affected by genetic diseases. Without a commitment to ethical principles, we risk navigating the landscape of genetic medicine without the moral compass needed to guide our actions.
Cultural Sensitivity in Gene Editing Applications
As gene editing technologies become more mainstream, cultural sensitivity is paramount in their application and acceptance. Different cultures have varying beliefs about genetics and health, which can influence how communities perceive interventions like CRISPR. Engaging with cultural perspectives can enhance the acceptance of gene therapies, particularly in diverse societies where traditional practices may conflict with modern medical interventions.
Moreover, the narratives around conditions like sickle cell disease are often intertwined with cultural identity. Therefore, it’s vital to approach gene editing communications with respect and an understanding of these cultural contexts. By integrating cultural sensitivity into discussions, we can foster trust and collaboration, leading to greater acceptance and ethical use of gene editing technologies in diverse populations.
Future Directions for CRISPR Research
The future of CRISPR research is both exciting and complex, laden with potential breakthroughs that could enhance human health dramatically. As scientists explore the limits of gene editing, the field will likely expand into various areas of medicine, including the treatment of genetic disorders, cancer, and infectious diseases. Nevertheless, ethical considerations must remain at the forefront of scientific exploration.
Investment in research that addresses both the practical applications and the ethical implications of CRISPR is essential. Collaborative efforts between geneticists, ethicists, and public health experts can lead to innovations that are not only effective but also socially responsible. As we stand on the brink of a genetic revolution, a balanced approach that prioritizes ethical standards will be critical in ensuring the benefits of CRISPR technology are realized equitably.
Public Perception of Gene Editing Technologies
Public perception plays a significant role in the acceptance and implementation of gene editing technologies like CRISPR. Increasing awareness about the capabilities and limitations of these technologies is necessary to shape informed opinions among the populace. Public forums, educational initiatives, and discussions framed around the real-world implications of gene editing can demystify the science and address common concerns over safety and ethics.
Moreover, as the narratives around genetic interventions evolve, it is essential to foster dialogue that incorporates community voices, especially those affected by genetic conditions. Understanding public sentiment will help guide ethical frameworks that align with societal values and expectations. By actively engaging the community in the conversation about gene editing, we can build a foundation of trust and cooperation that will ultimately benefit everyone involved.
Regulatory Challenges in CRISPR Implementation
Regulatory challenges present a significant hurdle in the widespread adoption of CRISPR technology. The landscape of regulation is not uniform across countries, and the patchwork of laws can lead to confusion and potential misuse of gene editing. Clear guidelines are essential to govern the practice safely and ethically, ensuring that advancements in gene therapy align with public health goals and ethical considerations.
Additionally, the regulatory framework must adapt as the science progresses. Ongoing dialogue among scientists, policymakers, and ethicists is crucial to developing policies that reflect the current understanding of gene editing. Such collaboration can facilitate the creation of robust regulations that not only protect patients but also foster innovation within the field of genetic medicine.
Frequently Asked Questions
What are the ethical implications of CRISPR gene editing in medicine?
The ethical implications of CRISPR gene editing in medicine revolve around issues of consent, the potential for unintended consequences, and the societal impacts of gene editing technology. As CRISPR allows for both somatic and germline modification, ethical concerns arise regarding who makes decisions about modifications, particularly in cases where the traits being edited are not harmful. This can lead to discussions about health equity in gene therapy and whether these resources will be available to all.
How does CRISPR technology provide a potential cure for sickle cell disease?
CRISPR technology provides a potential cure for sickle cell disease by enabling the targeting and editing of specific genes responsible for the disease. Through somatic cell editing, scientists can remove the faulty genes that cause sickle cell anemia, effectively stopping the disease’s progression and alleviating symptoms. This method shows promise in improving patients’ quality of life, illustrating CRISPR’s transformative potential in treating genetic disorders.
What role does bioethics play in CRISPR gene editing?
Bioethics plays a crucial role in CRISPR gene editing by addressing the moral and ethical dilemmas associated with genetic manipulation. Issues such as consent, the potential for designer babies, and the long-term effects on human genetics must be carefully considered. Discussions in bioethics guide policies on how CRISPR technology should be applied, ensuring that advancements in gene editing respect individual rights and promote health equity.
What are the health equity concerns related to CRISPR technology and gene therapy?
Health equity concerns related to CRISPR technology and gene therapy include access to innovative treatments and the risk of widening existing health disparities. If gene editing treatments, such as those for sickle cell disease, are prohibitively expensive, the wealth gap could lead to unequal access. Ensuring that advancements in CRISPR technology benefit all populations and do not exacerbate inequalities is a critical consideration for health equity in gene therapy.
Why is there controversy around using CRISPR for conditions like Down syndrome?
The controversy around using CRISPR for conditions like Down syndrome stems from ethical questions regarding ‘editing’ human attributes that are compatible with life. Critics argue that deciding to modify genes for non-life-threatening conditions could lead to a slippery slope of gene editing based on parental preferences rather than medical necessity. This raises important discussions about the limits of gene editing, individual rights, and societal values, highlighting the need for careful ethical deliberation.
| Key Point | Details |
|---|---|
| The Ethical Dilemma of CRISPR | The debate centers on whether we should change human differences, with concerns about who decides what to edit. |
| CRISPR’s Potential | CRISPR allows modifications to both somatic and germline genes, potentially curing diseases like sickle cell anemia. |
| Cost and Accessibility | The high cost of treatments (e.g., $2.2 million for sickle cell) raises questions about health equity and who can access these technologies. |
| Health Justice Concerns | The advancement in gene editing could exacerbate inequalities, leading to more disparity in health outcomes. |
| Parental Decision-Making | The choice for parents to alter traits in their children raises ethical questions about authority and consent. |
| Oversight and Global Issues | Concerns about the illegal practice of gene editing in places without strict regulations, impacting global health safety. |
| Unintended Consequences | Modifications may lead to unforeseen health effects, as genes work in complex interactions beyond initial alterations. |
Summary
CRISPR gene editing presents a revolutionary opportunity to alter human genetics for health improvements, such as curing diseases like sickle cell anemia. However, the intricate ethical dilemmas and potential societal repercussions demand careful consideration before widespread application. As debates around health equity, parental rights, and regulatory oversight continue, society must navigate these challenges to responsibly harness the benefits of CRISPR.