Alzheimer’s research is at the forefront of understanding the complex mechanisms driving this devastating neurodegenerative disease. Scientists like Beth Stevens, based at Boston Children’s Hospital, have illuminated the critical role of microglial cells, which function as the brain’s immune system. These cells not only clear away damaged cells but also prune synapses that are essential for neuron communication. However, improper pruning may contribute to Alzheimer’s disease and other neurodegenerative disorders, revealing a potential target for innovative Alzheimer’s treatment. By identifying biomarkers for Alzheimer’s, researchers can facilitate earlier detection and intervention, paving the way for transformative developments in healthcare.
Investigations into dementia and related disorders have significantly evolved, thanks to pioneering efforts in scientific research. The work of prominent neuroscientists sheds light on the intricate workings of the brain’s immune response, particularly focusing on cells known as microglia. These cells play a pivotal role in maintaining brain health by removing waste and regulating neuronal connections. However, when this pruning process malfunctions, it can lead to conditions such as Alzheimer’s, making the quest for effective Alzheimer’s treatment even more urgent. Understanding biomarkers for dementia will not only enhance diagnosis but also open new avenues for therapeutic interventions.
Understanding Microglial Cells in Alzheimer’s Research
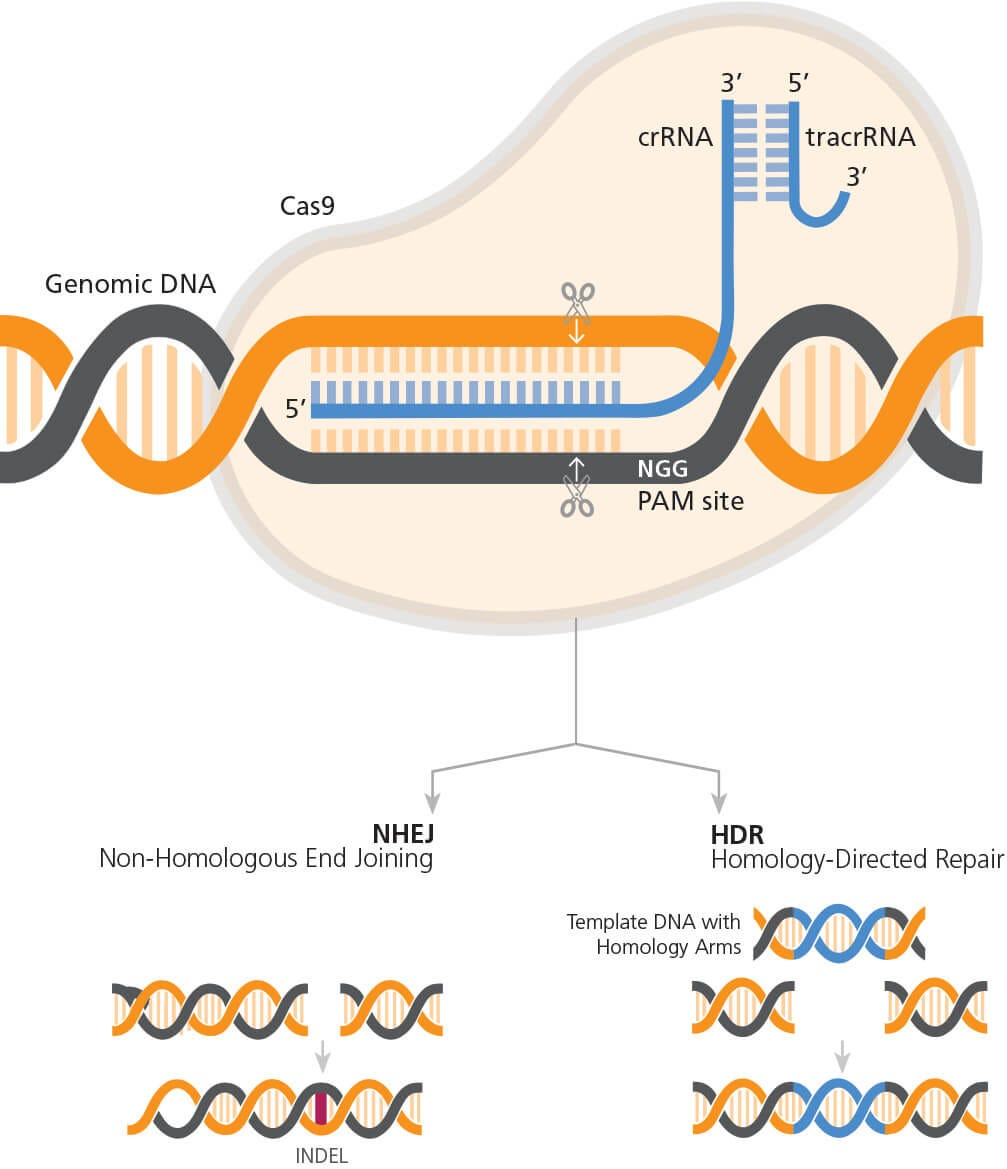
Microglial cells are an essential component of the brain’s immune system, playing a crucial role in maintaining neural health. In the context of Alzheimer’s research, these cells facilitate the clearance of debris caused by cell death and neuronal injury. However, recent studies conducted by Beth Stevens at Boston Children’s Hospital have revealed that improper functioning of these microglia can lead to neurodegenerative diseases, including Alzheimer’s. This dysfunction may disrupt synaptic pruning, which is vital for healthy brain function and communication among neurons.
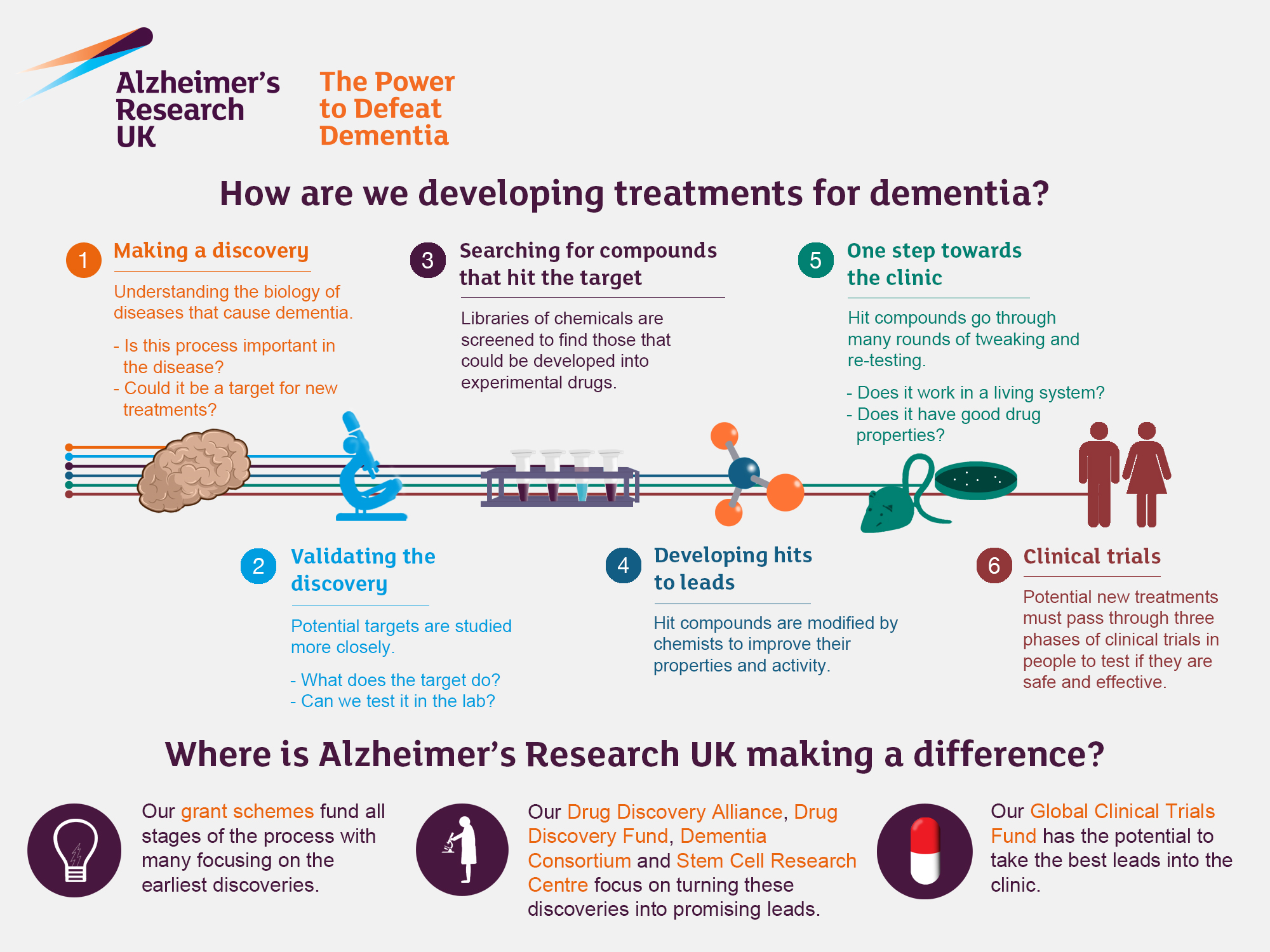
The implications of Stevens’ research on microglial cells extend beyond basic science. Understanding how these cells interact with the brain under pathological conditions could pave the way for innovative Alzheimer’s treatments. By identifying the mechanisms that lead to microglial dysfunction, researchers could develop therapies that restore their proper function, potentially halting or even reversing disease progression. The findings also highlight the importance of studying microglia in connection with other neurodegenerative diseases, as the insights gained may universally apply.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s research?
Microglial cells are crucial in Alzheimer’s research as they serve as the brain’s immune system. They monitor brain health by removing damaged cells and pruning synapses, a process that, when dysfunctional, can contribute to neurodegenerative diseases like Alzheimer’s. Research from the Stevens Lab at Boston Children’s Hospital has shown how improper microglial pruning can lead to the progression of Alzheimer’s and similar disorders.
How are biomarkers for Alzheimer’s being developed through current research?
Current Alzheimer’s research aims to identify new biomarkers that can facilitate earlier detection of the disease. The Stevens Lab has been pivotal in this field, utilizing insights gained from studying microglial cells to discover potential biomarkers. These advancements can help in diagnosing Alzheimer’s at a stage where interventions may be more effective.
What is the significance of neurodegenerative diseases in Alzheimer’s research?
Neurodegenerative diseases are significant in Alzheimer’s research because they encompass a range of disorders that affect the brain’s functionality, including Alzheimer’s itself. The understanding gained from studying these diseases, particularly through the analysis of microglial cell behavior, is essential for developing treatments and interventions that can improve patient outcomes.
What advances in Alzheimer’s treatment have resulted from recent research?
Advances in Alzheimer’s treatment have arisen from recent research focusing on microglial cells and their role in synaptic pruning. The insights from the Stevens Lab at Boston Children’s Hospital are paving the way for new medications aimed at addressing the underlying causes of Alzheimer’s, highlighting the importance of continued research in this area.
How is Boston Children’s Hospital contributing to Alzheimer’s research?
Boston Children’s Hospital is significantly contributing to Alzheimer’s research through the Stevens Lab, where scientists investigate the role of microglial cells in neurodegenerative diseases. This research is foundational in discovering how these immune cells can both protect and damage the brain, leading to potential new strategies for Alzheimer’s treatment and biomarker identification.
| Key Points |
|---|
| Beth Stevens, a neuroscientist, is pioneering research in Alzheimer’s disease by studying microglial cells, the brain’s immune system. |
| Microglia help clear damaged cells and prune synapses, but improper pruning can lead to neurodegenerative diseases like Alzheimer’s and Huntington’s. |
| The Stevens Lab’s findings could lead to new medicines and biomarkers for earlier detection of these diseases, impacting millions of Americans. |
| Stevens emphasizes the importance of foundational and curiosity-driven science which allows exploration into areas not possible with human studies. |
| Federal funding, especially from the NIH, has been crucial in supporting Stevens’ research efforts and advancing understanding in this field. |
Summary
Alzheimer’s research has entered a transformative era, thanks to leaders like Beth Stevens, whose groundbreaking work on microglial cells is reshaping our understanding of brain health. By uncovering the intricacies of these immune cells and their role in neurodegeneration, Stevens not only contributes to potential new treatments but also highlights the necessity of foundational research. In light of the expected doubling of Alzheimer’s cases by 2050, her findings are critical in addressing this growing health crisis. As we continue to follow the science, the path paved by innovative researchers provides hope for millions affected by Alzheimer’s.