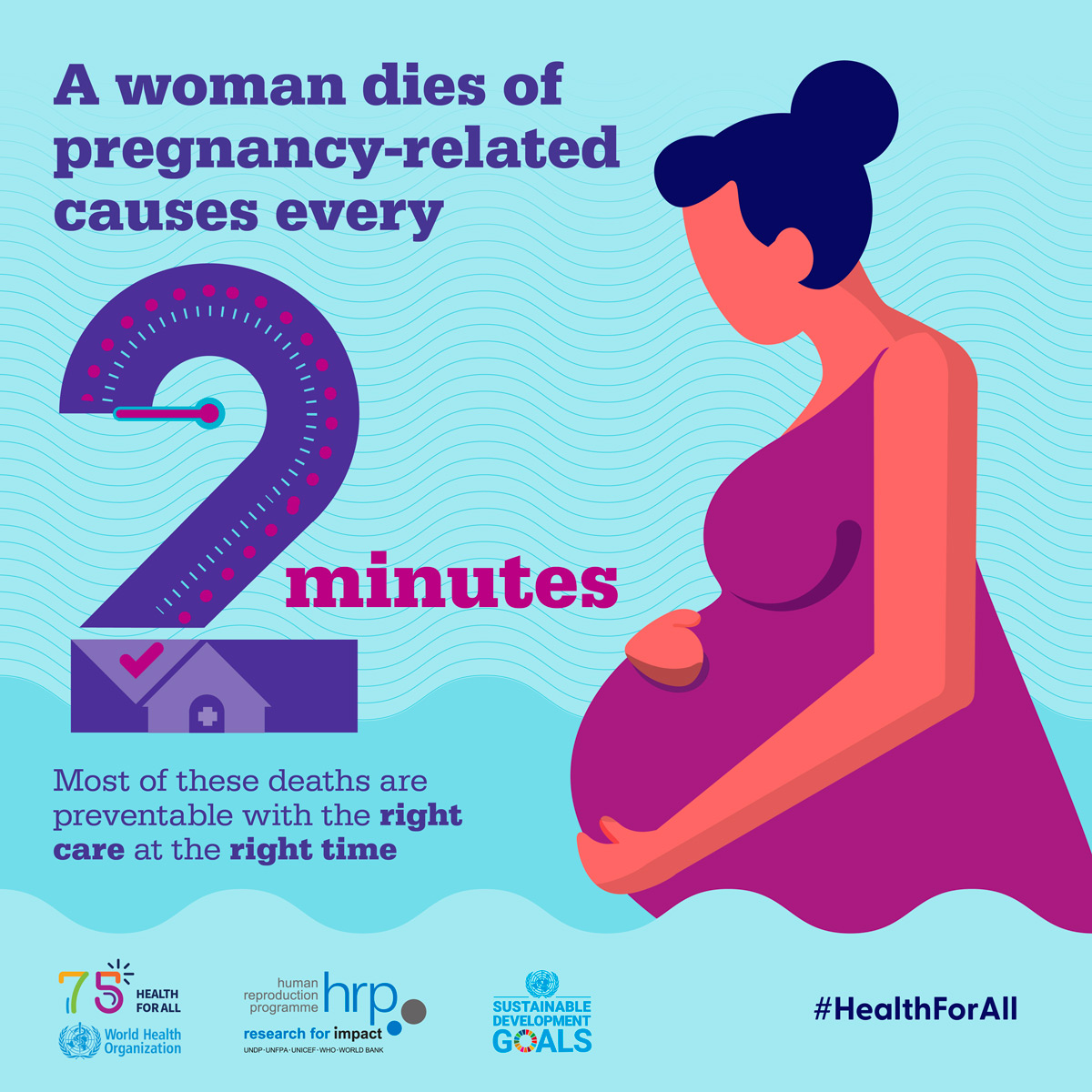
Maternal mortality remains a critical issue, as it reflects the tragic reality that pregnancy-related deaths are alarmingly high, particularly in the U.S., which leads its high-income peers in this area. Recent studies indicate that more than 80% of these pregnancy-related deaths could be prevented with improved maternal health services and better access to postpartum care. Racial disparities in maternal mortality rates reveal that American Indian and Alaska Native women experience the highest risk, highlighting a pressing need for equitable healthcare policies. The sharp increase in these rates, particularly during the COVID-19 pandemic years, underscores the vulnerabilities faced by expectant mothers, calling for urgent reforms in prenatal and postpartum care settings. Addressing preventable pregnancy deaths is paramount, as it not only saves lives but also significantly contributes to the overall health of communities.
The issue of maternal health, encompassing the safety of women during and after pregnancy, is steeped in urgency and complexity. Known for its far-reaching implications, the staggering rates of maternal mortality paint a somber picture of healthcare inequalities and systemic failures. Many health experts emphasize that these preventable pregnancy deaths often stem from inadequate prenatal support, insufficient postpartum care, and deeply ingrained racial disparities. As we strive to understand the nuances of this issue, it becomes increasingly clear that addressing healthcare access and quality is essential to ensure optimal outcomes for all mothers. By examining these factors closely, we can pave the way for significant improvements in the field of maternal health.
Understanding Rising Maternal Mortality Rates in the U.S.
The United States has been grappling with a disturbing trend as maternal mortality rates have climbed, making it the leader among high-income countries. Preliminary data indicates that from 2018 to 2022, the U.S. witnessed a rise in pregnancy-related deaths, predominantly contributing to this increased mortality rate. The research conducted by the National Institutes of Health highlights how factors such as economic disparities, inadequate access to quality prenatal care, and systemic biases have resulted in significant health risks for expectant mothers in the country.
One of the key insights from the study is the sheer number of preventable deaths linked to pregnancy complications. Over 80% of these fatalities could have been avoided if there was a more coherent healthcare policy in place, emphasizing effective prenatal care and equitable access to health services. This crisis necessitates urgent reforms to tackle the underlying causes, including ensuring accessibility to comprehensive maternal health services across diverse populations.
The Impact of Racial Disparities on Maternal Health
Racial and ethnic disparities are starkly reflected in the maternal mortality statistics, with American Indian and Alaska Native women facing the highest rates. The findings from the NIH report emphasize that non-Hispanic Black women also experience disproportionately high rates of pregnancy-related deaths, nearly three times higher than their white counterparts. This alarming disparity underscores a significant public health issue that requires immediate attention through targeted support and improved healthcare access for marginalized communities.
Furthermore, it is crucial to recognize the systemic factors contributing to these disparities. Issues such as socioeconomic inequalities, inadequate insurance coverage, and the historical context of discrimination in healthcare perpetuate these inequities, leading to poorer outcomes for women of color. Addressing these racial disparities in maternal mortality is not just about improving individual health outcomes but also requires a holistic approach that considers social determinants of health.
The Role of Postpartum Care in Reducing Maternal Mortality
Postpartum care is often overlooked in discussions about maternal health, yet it plays a pivotal role in ensuring safety and well-being for new mothers. Research indicates that late maternal deaths, occurring between 42 days to one year after childbirth, represent a concerning proportion of overall pregnancy-related deaths. The necessity for continuous and comprehensive postpartum support is highlighted by the data, indicating that many women experience preventable health complications during this critical period.
Improving postpartum care involves establishing a more extensive healthcare infrastructure that transcends the immediate postpartum period. It is vital that healthcare providers extend their engagement with mothers beyond the traditional six-week postpartum checkup, thus enhancing follow-up care. This comprehensive approach can contribute significantly toward reducing maternal mortality rates and ensuring healthier outcomes for mothers and infants alike.
Chronic Health Issues Contributing to Maternal Deaths
Chronic health conditions, particularly cardiovascular diseases, have emerged as a leading cause of pregnancy-related deaths in the United States. The trend suggests that more individuals are entering pregnancy with pre-existing health issues that complicate their maternal journey. This shift from hemorrhage to health complications underscores the pressing need for healthcare systems to prioritize chronic disease management and monitoring in pregnant individuals.
As the rates of chronic conditions like hypertension and pre-eclampsia continue to rise among younger populations, it is crucial to develop targeted intervention strategies focused on women’s health. By addressing these underlying health issues prior to and during pregnancy, healthcare providers can better mitigate associated risks, ultimately contributing to lower maternal mortality rates.
Policy Recommendations for Improving Maternal Health Outcomes
In light of the troubling trends observed in maternal mortality rates, it becomes essential to advocate for effective policy changes that prioritize maternal health. Research indicates that states with progressive maternal health initiatives, like California, demonstrate significantly lower mortality rates. This presents a viable model for other states seeking to enhance their maternal healthcare approaches and ultimately reduce preventable deaths.
To achieve substantial improvements, policymakers must invest in comprehensive maternal health programs that enhance access to services, education, and support for expectant mothers. By focusing on evidence-based practices and addressing barriers in healthcare access, it is possible to significantly reduce disparities and improve overall maternal health outcomes across diverse populations.
Integrating Mental Health Care into Maternal Health Services
Mental health is an essential, yet often neglected, dimension of maternal health. The postpartum period is characterized by a heightened risk for mental health disorders, including postpartum depression and anxiety. Recognizing and integrating mental health support into maternal healthcare services could radically improve outcomes for mothers, preventing a potential deterioration in physical health due to overlooked psychological challenges.
It is vital for healthcare providers to foster environments where mental health is prioritized alongside physical health, encouraging open discussions and providing resources for mental wellness. By incorporating mental health assessments and support into routine prenatal and postpartum care, healthcare systems can create a more holistic approach to maternal health, lowering the risk of adverse outcomes related to mental health.
The Importance of Comprehensive Healthcare for Expectant Mothers
Comprehensive healthcare during pregnancy is vital to mitigating risks that lead to pregnancy-related deaths. This encompasses not only regular prenatal consultations but also preventive care that addresses both physical and mental health. Providing an integrated healthcare system that prioritizes regular screenings for chronic diseases and mental health issues can significantly reduce pregnancy-related mortality rates.
Furthermore, it is essential to equip healthcare professionals with the tools and training needed to recognize red flags in maternal health more effectively. Continuous education on the unique needs of diverse populations, addressing both medical and social determinants of health, is critical to delivering quality maternal care.
Encouraging Community Engagement in Maternal Health Initiatives
Community engagement plays a pivotal role in enhancing maternal health outcomes, as it fosters awareness and supports resource accessibility for pregnant women. Hospitals and healthcare providers can collaborate with local organizations to create outreach programs that educate expectant mothers about available services. Such initiatives can empower women with vital knowledge about maternal health, thereby promoting proactive engagement in their care.
Moreover, community efforts can help dismantle the stigma surrounding maternal health issues, particularly those related to racial disparities. By fostering a supportive community environment, where women feel safe to share their experiences and challenges, healthcare systems can enhance overall health literacy and encourage utilization of maternal health resources, ultimately contributing to lower maternal mortality rates.
Advancing Research for Improved Maternal Health Policies
Advancing research is crucial in identifying effective strategies that can significantly improve maternal health outcomes. Ongoing studies help to unravel the complexities surrounding maternal mortality, allowing policymakers to tailor interventions based on empirical evidence. Establishing a robust maternal health research agenda will enable healthcare systems to better understand the factors contributing to maternal deaths and the specific needs of diverse populations.
Investment in research initiatives focused on maternal health not only informs policy reforms but also guides the allocation of resources toward effective programs aimed at reducing preventable pregnancy deaths. A continuous feedback loop between research findings and healthcare policies will ensure that maternal health services remain responsive and effective in addressing the evolving challenges in this field.
Frequently Asked Questions
What are the main causes of preventable pregnancy-related deaths in the U.S.?
In the U.S., the leading causes of preventable pregnancy-related deaths include cardiovascular diseases, hypertension, and complications like hemorrhage. Despite the high-income status of the country, over 80% of pregnancy-related deaths are deemed preventable, emphasizing the need for improved healthcare access and quality during pregnancy and postpartum care.
How does the U.S. compare to other high-income countries in maternal mortality rates?
The U.S. has the highest maternal mortality rate among high-income countries, with a significantly rising rate, particularly among racial and ethnic minorities. This disparity highlights systemic issues within the healthcare system and the need for policy reforms to address maternal health inequities.
What are the racial disparities in maternal mortality rates in the U.S.?
Racial disparities in maternal mortality are stark in the U.S., with American Indian and Alaska Native women experiencing the highest rates, followed by non-Hispanic Black women. The research indicates these inequities have persisted due to systemic barriers within healthcare access and quality.
What role does postpartum care play in reducing maternal mortality?
Postpartum care is crucial in addressing maternal mortality, as nearly a third of maternal deaths occur between 42 days and one year after childbirth. Improved healthcare systems that extend care beyond the six-week postpartum period can help prevent these late maternal deaths.
Why is it important to track late maternal deaths in relation to maternal mortality?
Tracking late maternal deaths is important as it recognizes that maternal health issues can persist well into the first year postpartum. This consideration calls for better healthcare responses and continuity of care to address potential complications that arise beyond the immediate postpartum period.
How can equitable policies impact maternal mortality rates?
Implementing equitable policies can significantly improve maternal mortality rates by ensuring access to quality healthcare for all women, particularly in underserved communities. Addressing financial, geographical, and social barriers can help reduce pregnancy-related deaths and disparities.
What innovative solutions can be implemented to improve maternal health outcomes?
Innovative solutions for improving maternal health outcomes include enhancing access to prenatal care, developing community health programs, and investing in education on pregnancy-related health issues. Policymakers and healthcare providers must collaborate to ensure quality care throughout pregnancy and postpartum.
What challenges impact the tracking of maternal mortality data in the U.S.?
Challenges in tracking maternal mortality data include variations in state reporting practices and the lack of a national system until recently. Improvements in data collection are essential for understanding the scope of maternal deaths and informing targeted interventions.
How does chronic disease prevalence affect maternal mortality rates?
The rising prevalence of chronic diseases, particularly hypertension and cardiovascular conditions, among younger populations can adversely affect maternal mortality rates. Increased awareness and management of these conditions during pregnancy are essential to mitigate risks.
What steps can be taken on a state level to address maternal mortality issues?
States can implement specific policies to improve maternal health, such as better funding for maternal care programs, addressing healthcare disparities, and promoting maternal health education. Tailored interventions can help states reduce their maternal mortality rates.
| Key Points |
|---|
| U.S. has highest maternal mortality rate among high-income countries, with a rising trend. |
| More than 80% of pregnancy-related deaths are preventable. |
| In 2022, maternal mortality was 32.6 deaths per 100,000 live births, an increase from 25.3 in 2018. |
| American Indian and Alaska Native women exhibit the highest mortality rate at 106.3 deaths per 100,000 live births. |
| Cardiovascular diseases are the leading cause of pregnancy-related death, surpassing previous leading causes such as hemorrhage. |
| Late maternal deaths account for nearly one-third of pregnancy-related deaths, indicating a need for better postpartum care. |
| The need for improved public health infrastructure and investment in maternal health care is critical. |
Summary
Maternal mortality continues to be a significant issue in the United States, as the country maintains the highest rates among high-income nations. This alarming trend highlights the critical need for enhanced prenatal care and ongoing support during the postpartum period. With the vast majority of these deaths deemed preventable, it is essential for healthcare policymakers to prioritize investment in maternal health initiatives. Addressing systemic inequities, improving healthcare accessibility, and enhancing public health infrastructures will be key in reversing the increasing rates of maternal mortality in the U.S.